This article first appeared in the Facebook Group Medical Monday.
Years ago, while taking my EMT-Intermediate class, we spent many hours on the application of MAST trousers (Medical Anti-Shock Trousers). We would apply these pants to patients that were severely hypotensive and, by providing circumferential pressure to the patients lower extremities, hopefully elevate their blood pressure. We spent hours learning how to apply them, hours learning how much to inflate and how to prevent them from deflating. We felt so strongly about them that they were part of the national exam. Yet when we went to the real world we found that removing them properly involved hours in the ER to avoid the sudden pressure drop from quick removal. Their use was causing additional harm. MAST trousers were relegated to the dustiest, darkest confines of the ambulance and were forgotten.
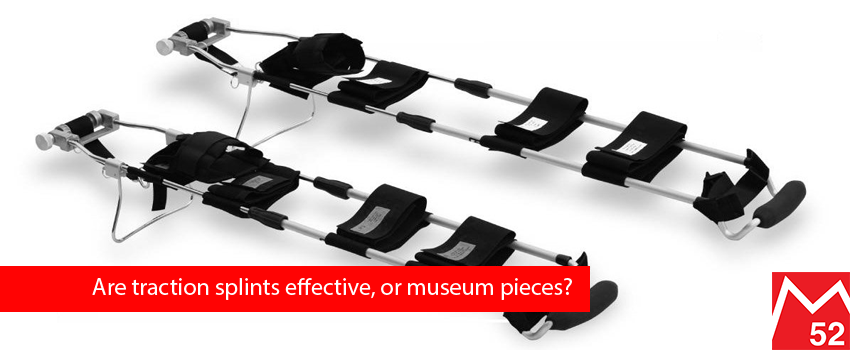
We still have equipment that is used because we think that they may work, yet there is no empirical evidence to their benefit. Traction splints are still carried on an ambulance and with patrols, yet are used without any proven relevant benefit.
When we went through class, we were taught that we would use traction splints for a patient that had a mid-shaft femur fracture; that it would reduce the patient’s pain and reduce the possibility for cutting the femoral artery with the jagged edges. We were told of the MANY contraindications to using the splint; injuries proximal or distal, injury to the femur that was too high or too low, osteoporosis, prior knee instability, pelvic injury. The fact is we spend an incredible amount of time spinning our wheels on a treatment that has no proven benefit, but many proven negative consequences.
The Femur is the largest, strongest bone in the human body and any trauma that can fracture this bone is significant. Without x-rays can we be certain that there are not additional injuries? The time that we take to properly apply the traction splint could be much better utilized by rapid transport to a hospital.
Consider also the length of the traction splint. By extending it several inches beyond the affected limb we essentially lengthen our patient. Ambulance cots and ski toboggans are created for patients generally shorter than 6’6”. In many instances the splint now extends beyond the end of the cot or transporting device. For a while we considered loading the patient backward on the cot, but by doing so we negated the design of the cot and ambulance or toboggan for a single piece of equipment that has questionable value.
Research of prior studies regarding the use of traction splints has shown a lot of opinion and very little objective evidence. Has the use of traction splinting been solely by conjecture?
We all agree that splinting is necessary for any instability of bones. We also agree that in all instances that we try to get the body back to as close to normal as possible. When a bone is broken, causing instability, we create a “fake bone” or splint to stabilize the affected area. But, does this benefit correlate to traction splinting?
Let’s do an experiment; break a pencil in two and then try to realign the ends. Don’t push them together; but by holding the pencil from the distal ends keep them closely aligned but apart. Now walk across the room while concentrating on keeping the two ends in line. Could you do it? Likely not. When we apply traction to a long bone, we are essentially trying to do the same thing; hold the ends apart, yet keep them in-line. The splint intentionally separates the limb from the rigid components to allow this alignment to maintain. In the Sager version the rigid “splint” is far too weak to provide any stabilization. We place the patient in an ambulance with the traction applied and drive down a road, How well do you think that these bones stay aligned? Now, let’s try a different way. After breaking the pencil, I’d like you take another pencil and place it next to the broken one and secure it in multiple places with tape, but not directly over the break. Recreate the walk across the room and notice the movement of the broken pencil, which is likely much less. The rigid splint provides a much more stable support for the break and reduces movement.
Shall we also consider the number of times that a traction splint can surpass all of the contraindications and be used? In my 20 year career, I’ve had only 1 patient whose injuries would allow the use of a traction splint. While doing dishes, he heard a loud popping sound in his leg and instant pain. He hobbled to the garage to take his car to the hospital. He found the pain insurmountable, and called an ambulance. His description of the incident led us to believe that he dislocated his knee. Upon visualization we found a stable knee but a 30 degree angulation mid-shaft. The patient was given a strong pain killer and we applied the traction splint. When we were taught to apply a traction splint we were told to tighten until you could “see the relief on the patient’s face.” I only saw relief when I stopped turning and the pain killer took hold. In fact the traction caused more pain during application. This was an atypical injury and this gentleman’s new bone cancer diagnosis.
The first traction splint was designed by John Hilton in 1860 and later modified by Hugh Owen Thomas, a British orthopedic surgeon, in 1875. It was one of the first required tools on ambulances in the 1950’s (even before oxygen). A lot of time is spent learning and relearning traction splinting. Theoretically the idea of pulling the bones apart makes sense, but in all of its years of use there has yet to be a single study noting benefit to the morbidity of the patient over standard splinting. There have been a couple of studies, done overseas, that show that traction splints do show a reduction in pain, but no difference in the long-term use of the limb. Conversely there have been studies done that show that for every 10 degrees of angulation of the foot, off of 90, that there was an additional week required of PT to return to normal function. Unfortunately the ability to get a statistically significant sample of solely femur fractures will prevent ever being able to do effective double blind studies. If one has to wait over 20 years to see their first acceptable patient for inclusion, how long would we wait to have a significant number to compare?
A few years ago the company that I work for decided to create a “museum” of old equipment; MAST trousers, early cardiac monitors, latex etc. It made me feel old to realize that I’ve been doing this long enough to have used each of these pieces of equipment. Perhaps it’s time to move the traction splint to this “museum” and make us all feel like old dogs.
Sources: http://www.emsworld.com/article/11542786/traction-splint-evidence-and-efficacy
Photo: alibaba.com
1 Comment
I'm not yet ready to ditch it. True, there are few studies that really cut the mustard to support it, and it's application is limited. However I have seen it work to bring relief to a grievously injured skier, and have from patrol-mates heard of others. In an area of practice where analgesia of the strength needed to placate such a patient is often an hour or more away, there's very much an ongoing role for this treatment. If you feel the need to supplement the sager's traction with splinting to the device, that can be easily done -- but is rarely necessary with an appropriately handled patient.
For the right injury, the right instrument. Just like a backboard: don't chuck it just yet. Only try to be judicious in how and when you use it.
Leave A Comment